.png)
Jump to section
Achilles tendinopathy causes pain at the back of the heel. It’s caused by damage to the Achilles tendon, either right where it attaches at the back of the heel or slightly further up the tendon. Achilles pain is among the most common problems our podiatrists see and treat at our Brisbane CBD and Newmarket clinics.
Your Achilles tendon is the largest tendon in your body. It connects the muscles in the back of your calves to your heel bone. Your Achilles tendon allows you to stand on your toes and push off the ground when walking, running or jumping. You wouldn’t be able to walk without it, so looking after your Achilles and managing any niggles before they turn into an injury is always important.
There’s a condition similar to Achilles tendinopathy called Achilles tendonitis. Although people may use the terms interchangeably, Achilles tendinopathy and Achilles tendonitis are different conditions.
Achilles tendinopathy is classified as either mid-portion or insertional depending on the location of the injury.
Much like the two different types of Achilles injuries above, it's also important to diagnose the correct type of tendinopathy as many of the exercises for mid-portion will aggravate an insertional condition if misdiagnosed. This is where working with a podiatry team like ours who are highly experienced in managing Achilles pain is essential.

Achilles tendinopathy develops gradually from overloading and stress on the Achilles tendon. While age can play a role, it's more about the tendon wearing down from repeated activities, whether in your job, exercise routine, or daily life. We most often see Achilles tendinopathy in adults aged between 30-50 who exercise at least semi-regularly.
Achilles tendinopathy is considered a degenerative condition, which means the tendon fibres start to break down and lose their strength over time. Small tears and damage occur when the strain from these activities exceeds what the tendon can handle. In more severe cases, this can lead to partial tears or even a complete rupture of the tendon.
The most common causes of Achilles injuries our podiatrists see and treat include:
In many cases we see, a patient may experience dull aches or niggles at the back of the heel and ignore these early signs in the hopes that the pain will resolve on its own. Unfortunately, without changing whatever is causing the overloading, the damage will progress, and significant pain and injury will eventually occur.
You don’t have to be physically active to develop an Achilles injury, although it does tend to be a more common issue for people who take part in running-based exercise and stop-start sports, including tennis, netball, soccer, long-distance running, and the like.
Achilles injuries affect both men and women, with evidence showing it is more common among men over the age of 30. Factors that can raise the risk of someone developing Achilles tendinopathy include:
Symptoms of Achilles tendinopathy can vary in people, with some common signs including:
If you're experiencing pain in the back of your heel the morning after activity, there are a couple of things you can do yourself.
P = Protection
The first thing you should do when you injure your Achilles tendon is to rest the injured tendon and
reduce any weight and pressure on the area. During this time, you may use assistive devices, like crutches, to help you walk and NSAIDS for
pain relief and anti-inflammatory properties.
OL = Optimal loading
With any movements involving muscles or tendons, if you don’t use it, you lose it! These
rings true even in the case of an injury. While maintaining protection, you should be able to progress from a few days of rest, to gentle
exercises. This progressive loading will help to promote healing and prevent muscle atrophy (where your muscles lose strength).
I = Ice
Ice the tendon with an ice pack wrapped in a towel for 15-20 minutes at the end of the day. This provides pain
relief and reduces inflammation and swelling surrounding the tendon. You can also do this several times per day throughout the day.
C = Compression
While icing the tendon, you can also add compression with bandages to assist in reducing the swelling
surrounding the tendon — but be careful not to wrap it too tight.
E = Elevation
Raise your legs above the level of your chest. When the legs are higher than the heart, the blood will
flow back to the heart faster, which will reduce swelling. It is easy to do by putting your legs over a pillow while you're lying down.



Tight calf muscles are one of the major contributors in developing Achilles tendon issues. When we start exercising with tight calves, this
places greater stress on the Achilles tendon. As you continue exercising, the level of stress that the Achilles is exposed to will likely
exceed its normal threshold, which ultimately leads to tendon breakdown.
When is a good time to start stretching?
The timing to start stretching is very important when dealing with Achilles tendon issues. You want to start the stretching process as soon as you can to decrease the stress on the tendon, but doing so too early may lead to further injury.
We generally recommend the following:
Some stretching exercises include:
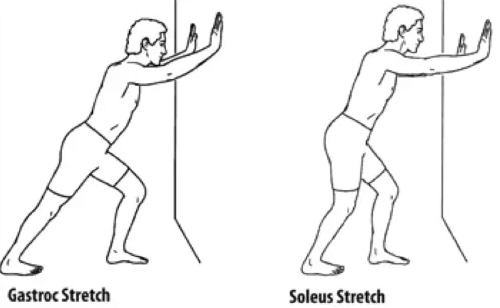
Wall Calf Stretch
Gastroc stretch: Position yourself facing the wall.
Keep the leg to be stretched at the back and the forward leg bent. Lean forward until you can feel the calf stretch in the back
leg.
Soleus stretch: Same positioning as previous stretch. The only difference is bend both the back and front leg. You should feel the stretch in the lower part of the calf.
Hold the position for 30s and repeat it 3 times for each leg.

Calf foam rolling
Start off foam rolling gently in long strokes from the top of the calf to the bottom. Once the calf is warmed up, move to a spot of
tenderness and hold the area for 20s. Once the area is finished you can then move on to the next. One technique you can use to increase the
effectiveness is that while you are on the spot of tenderness, you can then move the ankle up and down.
Often when people experience pain in their feet or legs, their first response is to stay at home and avoid doing all forms of activities in an attempt to heal the area. Although resting is helpful, it can’t be all you’re doing, and it shouldn’t be done for too long. This is as progressively loading your Achilles is crucial for its recovery.
Picture a rubber band. If the load being placed on the rubber band is stronger than its elasticity, the band will snap. Your Achilles is similar. If the load and forces acting on the tendon are greater than its elasticity and how much load it is able to safely handle, it will begin to tear. However, if a gradual load is applied to the tendon without reaching the breaking point, the tendon will adapt to the load applied and become stronger and more tolerable to higher loads.
The key word here is progressive. Going too hard too fast is one of the worst things you can do, and will quickly lead to a worse injury.
To start things off, if you are experiencing high levels of pain, and unable to perform any dynamic loading of the tendon, you can start by
doing some isometric exercises.
.png.png)
Depending on the symptoms and tendon irritability, this exercise can be performed with either one or both legs.
If you are able to tolerate dynamic loading with minimal pain levels, you can start introducing some additional load into the tendon
through:
| Exercises |
Protocol |
| 1. Seated Calf Raises |
3 sets of 10 reps |
| 2. Double Leg Calf Raises |
3 sets of 10 reps |
| 3. Single Leg Calf Raises (with weights) |
3 sets of 10 reps |
Do you feel your Achilles tendon is sometimes worse when you go for your usual stroll around the park in Dunlop volleys, or go to work in your ballet flats? Why is that?
Alongside the level of support in the shoe, it is also based on the pitch of the shoe.
The pitch of the shoe, or the “heel drop”, refers to the differences in height from the rearfoot to the forefoot. The major similarity between the shoes mentioned above is the lack of heel pitch. This can increase the level of discomfort felt in the tendon, especially if your calves are tight.
One of the first things you can change is your shoes. Most traditional running shoes have a shoe pitch of 10-12mm. This tends to increase the level of your discomfort as it reduces the stress on the Achilles tendon by elevating the heel towards the calf muscle.
If you are already in good, supportive running shoes, your podiatrist may recommend using either prefabricated or custom-made heel lifts. We have these available in our clinic. You place these in the heel region of your shoe, preferably under the innersole, to offset the adverse effects of tight calf muscles and Achilles tendons.
Hopefully, by now, you will be more confident in knowing what Achilles tendinopathy is and have learned a few tips to help you get back on
your feet quicker. However, to get your Achilles pain gone for good and your injury successfully rehabilitated for the long term, there are
several proven treatments to help. What you will benefit most from will depend on the results of your assessment with us.
At The Feet People, we use custom foot orthotics to successfully treat a range of foot and leg conditions, which very much includes Achilles tendinopathy. Custom foot orthotics are podiatrist-prescribed, custom-designed insoles, which we manufacture and fit into your shoes. This includes running shoes, work shoes, and day-to-day walking shoes. The primary function of orthotics is to distribute the pressure evenly across your foot, modify the load and forces your feet and legs are exposed to, and help correct your unique biomechanical misalignments or malfunction to improve your foot function and performance.
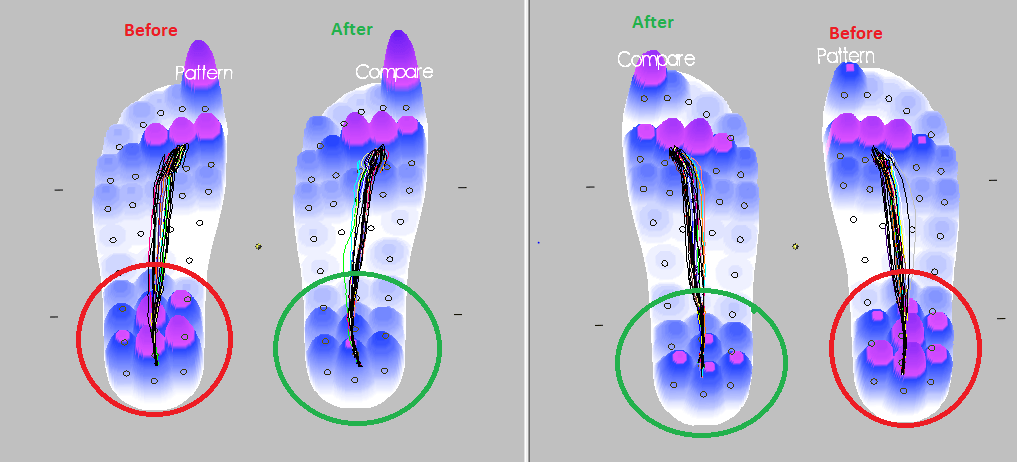
ParoTec in-shoe pressure analysis system
We also use the ParoTec pressure analysis system, which accurately measures the pressure through the feet when performing dynamic movements.
This is a great way to show the effectiveness of the therapies we use, and is a great guide to see if you could benefit from additional
support in certain areas.
Shockwave treatment
(ESWT)
For long-standing Achilles tendinopathy issues, shockwave is a fantastic treatment. Shockwave works by emitting acoustic waves into the Achilles tendon by applying the shockwave handpiece to the skin. These pressure waves will effectively increase the blood flow to the area (essential for healing and repair) and promote the formation of new blood vessels to create an improved environment for tissue repair.
The MLS laser is a proven, painless and safe way to relieve pain, reduce any inflammation present with your Achilles injury, and support the repair of your Achilles tendon. It works by interacting with the cells to help restore normal, healthy function. When the body can work optimally, it is in the best position to be able to heal and repair effectively. Learn more about how the laser works here.
Stretching and strengthening program
Tight calf muscles are one of the significant contributors to Achilles tendon pain, so having a stretching program that addresses this issue (if present) as well as other muscle tightness, weakness or imbalance will help you both manage your current symptoms and help prevent the problem from recurring in the future. Our podiatrists will create a professional progressive loading plan, allowing you to apply a safe, gradual load to the tendon without going overboard and causing more damage. This will result in gradual and safe strengthening and a return to healthy tendon function.
If the stretching exercises are not producing any short-term benefits, dry needling uses fine, medical-grade needles to address calf tightness effectively, helping to improve the range of motion at your ankle quickly to best support your recovery.
Foot mobilisation is a great way to address any dysfunction and stiffness in the feet, helping promote optimal movement so you can recover faster. It can also improve your overall gait and performance, as well as help reduce the likelihood of your Achilles pain returning in the future.
It may not be possible to prevent Achilles tendinopathy completely, but there are a number of preventative measures you can take to reduce your risk.

Our feet are the foundation for the entire body, so it's important that they have enough strength to tolerate our activity levels. Use
these three exercises to help strengthen your feet.

Not everyone needs orthotics, but they can play an integral role in treating or relieving pain in several foot and lower limb conditions.

The heat and humidity of an Australian summer makes it a prime time for issues to arise, so our newest podiatrist Lucy has put together
seven helpful tips to keep your feet healthy and problem free throughout summer.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | 7:40am - 2:00pm |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051