
Jump to section
Plantar fasciitis heel pain is one of the top conditions seen and treated by our podiatrists. As such, we’ve developed extensive evidence-based processes paired with gold-standard techniques and technologies to relieve your heel pain and reduce the risk of it returning in the future.
You have a thick band of connective tissue at the bottom of your foot called the plantar fascia. It starts from your heel and extends to your toes in the shape of a fan. The plantar fascia is very important for healthy, pain-free foot movement, helping to stabilise and support your foot through any activities you do. When it becomes overloaded, the plantar fascia can become injured. That’s when pain and inflammation start, which is your body’s way of letting you know something is wrong. When you have an injured and sore plantar fascia, this is known as plantar fasciitis.
Our podiatrists often see this injury after something changes in a person’s daily habits, activities or training regime. Plantar fasciitis is chronic (long-lasting), as the plantar fascia has to repeatedly and constantly deal with a load that it cannot manage from your daily activities.
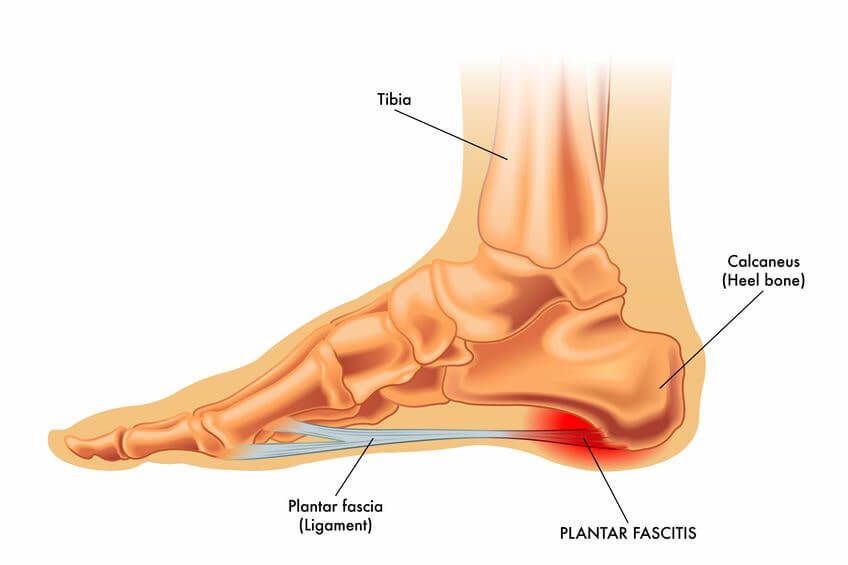
It is not uncommon for heel spurs to occur at the same time as plantar fasciitis due to the stress and strain the heel bone is being placed under. Hence, many people often think that heel spurs must be the cause of their heel pain, or even that ‘plantar fasciitis’ and ‘heel spurs’ are the same thing. This is actually not the case! As confirmed by research, most heel spurs are asymptomatic and don’t cause pain in the plantar fascia tissue. Instead, it’s a damaged fascia that’s the cause of the pain.
Heel spurs being the cause of heel pain is one of the top heel pain myths we hear - you can read our list of heel pain myths and the truth about them here.
As mentioned above, the most common cause and risk factor for plantar fasciitis is a change in how you load your foot - in a way that leaves it overloaded.
When repetitive, high loads are placed on the heel bone and the connecting soft tissues and structures, they are constantly fatigued. They get tired! And overworked. This result means their ability to absorb the excessive shock forces plummets, leading to inflammation and injury (plantar fasciitis).
Your risk of developing plantar fasciitis is often a combination of the following factors:
Plantar fasciitis symptoms can be quite debilitating, especially as it continues or worsens. The pain is typically localised to the heels, although it may radiate into the arch. You feel the most pain and discomfort when you take your first steps after waking in the morning or after standing after putting your feet up to rest for a while in the evening.
Other symptoms of plantar fasciitis heel pain can include:
The signs and symptoms of plantar fasciitis closely resemble those of other causes of heel pain, so it's important to get a correct diagnosis from experienced podiatrists who are familiar with the condition so that you get the right treatment.To diagnose the cause of your heel pain, we start with a complete physical assessment of the area. This includes evaluating your foot posture, muscle strength and imbalances, joint flexibility testing, checking your gait via video gait analysis, and further specialised assessments as needed based on the results we find.
In some cases, ultrasound imaging may be used to confirm the diagnosis or to assess the extent of the injury's damage. This tends to
only be in cases where we suspect you have multiple injuries at once, or your pain is particularly severe, and we suspect there may be a
significant tear in your plantar fascia that we’ll need to offload and closely monitor.
Plantar fasciitis is one of the most common conditions that our podiatrists see in our Brisbane CBD and Newmarket clinics.
When treating plantar fasciitis, we often suggest a personalised combination of the following treatments to allow you to achieve the fastest and most effective recovery.
Your pain levels and symptoms are likely to improve in a few days or weeks simply by resting, but this doesn’t stop the problem from returning once you start being active and spending whole days on your feet again. This is why a comprehensive treatment plan is needed that includes stretching and strengthening the muscles around the feet and legs, so the problem doesn’t keep returning and troubling you on and off for years.
While you may not be able to “fix” plantar fasciitis to get long-term relief at home, there are definitely things you can start doing at home today to support your recovery and help bring relief.
Strength exercise - Calf raises with a twist.
Self massage


Plantar fasciitis is not an injury where you can ignore the pain until it gets better. The longer you leave it untreated, the longer the
recovery period. Without making any changes to your routine, the pain and injury will continue to get worse until you end up possibly
tearing or rupturing the plantar fascia. If this happens, you'll generally require extended periods in a moon boot.
You shouldn't wait to experience pain before making changes to your lifestyle that would help prevent plantar fasciitis. Here are several simple preventative measures you can implement to help reduce your risk of developing this injury.

If you are injured and experiencing heel pain, the first thing you should do is look at your activity levels and modify them if needed.
Follow these three simple rules to help manage your heel pain

Not everyone needs orthotics, but they can play an integral role in treating or relieving pain in several foot and lower limb conditions.

The heat and humidity of an Australian summer makes it a prime time for issues to arise, so our newest podiatrist Lucy has put together
seven helpful tips to keep your feet healthy and problem free throughout summer.
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:00pm |
| Friday | 7:40am - 2:00pm |
| Saturday | CLOSED |
| Sunday | CLOSED |
Ground Floor, 344 Queen Street,
Brisbane City QLD 4000
| Monday | 7:40am - 6:00pm |
| Tuesday | 7:40am - 6:00pm |
| Wednesday | 7:40am - 6:00pm |
| Thursday |
7:40am - 6:30pm |
| Friday | 7:40am - 5:00pm |
| Saturday | 7:40am - 4:30pm |
| Sunday | CLOSED |
Newmarket Village, 114/400 Newmarket Rd, Newmarket QLD 4051